To become a BCBS provider, you'll need to complete their onboarding form process, which involves several steps and requirements. The process typically starts with submitting the BCBS provider onboarding form.
The form requires providers to provide their business and contact information, including their National Provider Identifier (NPI) and Taxpayer Identification Number (TIN). This information is used to verify the provider's identity and credentials.
Providers must also provide their practice details, such as their specialty, location, and services offered. This information helps BCBS to determine the provider's eligibility and scope of participation in the network.
Provider Onboarding Process
The provider onboarding process is a crucial step in becoming a part of the Blue Cross Blue Shield network. To start, you need to complete the Provider Onboarding Form, which will ask for various details about your practice.
Providers who want to be in-network will have additional fields to complete on the form, but don't worry if you need help – you can select the question mark icon where available. This will provide you with assistance in filling out the necessary information.
Here are the steps to complete the Provider Onboarding Form:
- Complete the Provider Onboarding Form
- Providers who want to be in-network will have additional fields to complete
- Providers can select the question mark icon for assistance
Recredentialing
Recredentialing is a crucial step in maintaining your provider status with BCBSMT. It's performed every three years to ensure your credentials are up-to-date.
You'll need to finalize your Council for Affordable Quality Healthcare (CAQH) application within 45 days to avoid starting the credentialing process over. Failure to do so will cause the process to be discontinued.
The CAQH application is important to complete accurately and efficiently to avoid delays. It's essential to keep track of your deadlines to avoid any issues.
If you're unsure about the recredentialing process, you can refer to the BCBSMT website for more information.
Updates
Credentialing updates are a crucial part of the onboarding process. Keeping your information current with organizations like CAQH and BCBSMT is your responsibility.
You'll need to regularly update your credentials to ensure accuracy and completeness. This might involve submitting new documentation or verifying existing information.
Staying on top of updates will help prevent delays and ensure a smooth onboarding experience.
For Professional Providers
For Professional Providers, the provider onboarding process is a bit more involved. You'll need to complete the Provider Onboarding Form, which is the first step in the process.
If you don't already have a Provider Record ID established with BCBSTX that matches your billing information, you'll need to complete the form. This includes your Rendering NPI, Billing NPI, and TIN.
A complete signed, and dated W9 is required with all new group and solo practitioner Provider Onboarding Form submissions. You'll also need to provide a copy of each provider's license.
Here are the key requirements for Professional Providers:
- Provider Onboarding Form completion
- Matching Provider Record ID with billing information (Rendering NPI, Billing NPI, and TIN)
- Completed and signed W9
- Copies of each provider's license
Group Providers
As you go through the provider onboarding process, you'll need to focus on group providers. To get started, complete the Provider Onboarding Form using the group information.
Make sure to only send new providers, not a full roster, if you're an existing group. This will help streamline the process.
You'll need to download and submit the required Provider Roster in the provided format. This is an important step, so don't skip it.
Here are the key steps for group providers:
- Complete the Provider Onboarding Form with group information.
- Only send new providers, not a full roster, if you're an existing group.
- Download and submit the required Provider Roster in the provided format.
- Use one Tax ID per onboarding request.
BCBS of Texas Process
The BCBS of Texas process is designed to be user-friendly and efficient. To get started, you'll need to complete the Provider Onboarding Form.
This form is the first step in the credentialing process. You'll need to submit required documentation, including a signed W9 and copies of your licenses, to get in-network status.
Providers can select the question mark icon on the form where available if they need assistance with certain fields. This is a helpful resource for those who may be unsure about what information is required.
Here are the steps to complete the Provider Onboarding Form:
- Complete the Provider Onboarding Form
- Providers who want to be in-network will have additional fields to complete on the form
- Providers can select the question mark icon where available if they need assistance with those fields
By following these steps, you'll be well on your way to getting in-network with BCBS of Texas.
Application and Status
The CAQH standardized application is an online form that meets the needs of all participating health care organizations. You'll need to indicate which participating health plans and health care organizations you authorize to access your application data.
The online CAQH application can be completed at any time, and it's one step of the Join Our Network onboarding process. A current, complete credentialing application through CAQH is a requirement to begin the credentialing portion of onboarding.
To check the status of your credentialing process, enter your NPI or license number in the Credentialing Status Checker. This will give you an update on the progress of your credentialing.
Completing the Application
Completing the application process is a crucial step in becoming part of the network. The CAQH standardized application is an online form that meets the needs of all participating health care organizations.
To complete the application, you'll need to indicate which participating health plans and health care organizations you authorize to access your application data. Learn more about the CAQH application process.
You can complete the CAQH application at any time, and it's an essential step in the credentialing process. A current, complete credentialing application through CAQH is a requirement to begin the credentialing portion of onboarding.
If you're a provider, you'll need to register online and complete the Council for Affordable Quality Healthcare Proview credentialing application. If you're already registered with CAQH, you can log in and update any outdated information.
Here are the steps to complete the credentialing process:
- Credentialing Process for Physicians and other Professional Providers: Register online and complete the CAQH Proview credentialing application.
- Credentialing Process for Hospitals and other Ancillary Providers: (Details not provided in the article section)
Additionally, BCBSMT will provide a provisional credentialing process, which allows for a provisional network participation status if you have:
- A valid BCBSMT Provider Record ID for claim payment
- Completed CAQH ProView database online application with "global" or "plan specific" authorization to BCBSMT
- A valid license to practice in Montana
- Ensure Your Montana Practice Address is provided and marked as the Primary Address
- Ensure the malpractice Certificate of Insurance includes the individual provider's name
Status Checker
You can easily track the progress of your credentialing process through our online tool. To do this, simply enter your NPI or license number into the Credentialing Status Checker.
Our Credentialing Status Checker is a convenient way to stay informed about the status of your credentialing application.
Key Information
Medical credentialing is crucial for healthcare providers to accept third-party insurance patients and increase their collection.
In the healthcare industry, medical credentialing is essential for compliance with regulations, which often involves communicating with insurance providers.
Providers who don't prioritize credentialing may struggle to get paid by insurance companies.
Credentialing services help healthcare providers navigate the process of submitting required documentation to payers and credentialing verification organizations.
This process is particularly important for group physicians, solo physician offices, and ambulatory surgical care facilities.
Frequently Asked Questions
How long does it take to get credentialed with BCBS TX?
CAQH credentialing applications are typically reviewed within 8-10 calendar days. Contact your local Network Management Office for more information and to track your application status
What is the difference between blue cross, blue shield, and blue cross?
Blue Cross and Blue Shield are two separate entities, with Blue Cross covering hospital services and Blue Shield covering physician services. Blue Cross refers specifically to an association of health insurance plans in the US, not a single entity.
Sources
- https://www.bcbsmt.com/provider/network-participation/network/how-to-join
- https://www.medicalbillersandcoders.com/blog/how-to-credential-a-group-practice/
- https://www.bcbsilcommunications.com/newsletters/br/2019/sept/the_provider_onboarding.html
- https://www.bcbsok.com/provider/network/credentialing.html
- https://www.bcbsmt.com/provider/network-participation/network/how-to-join/steps-to-join
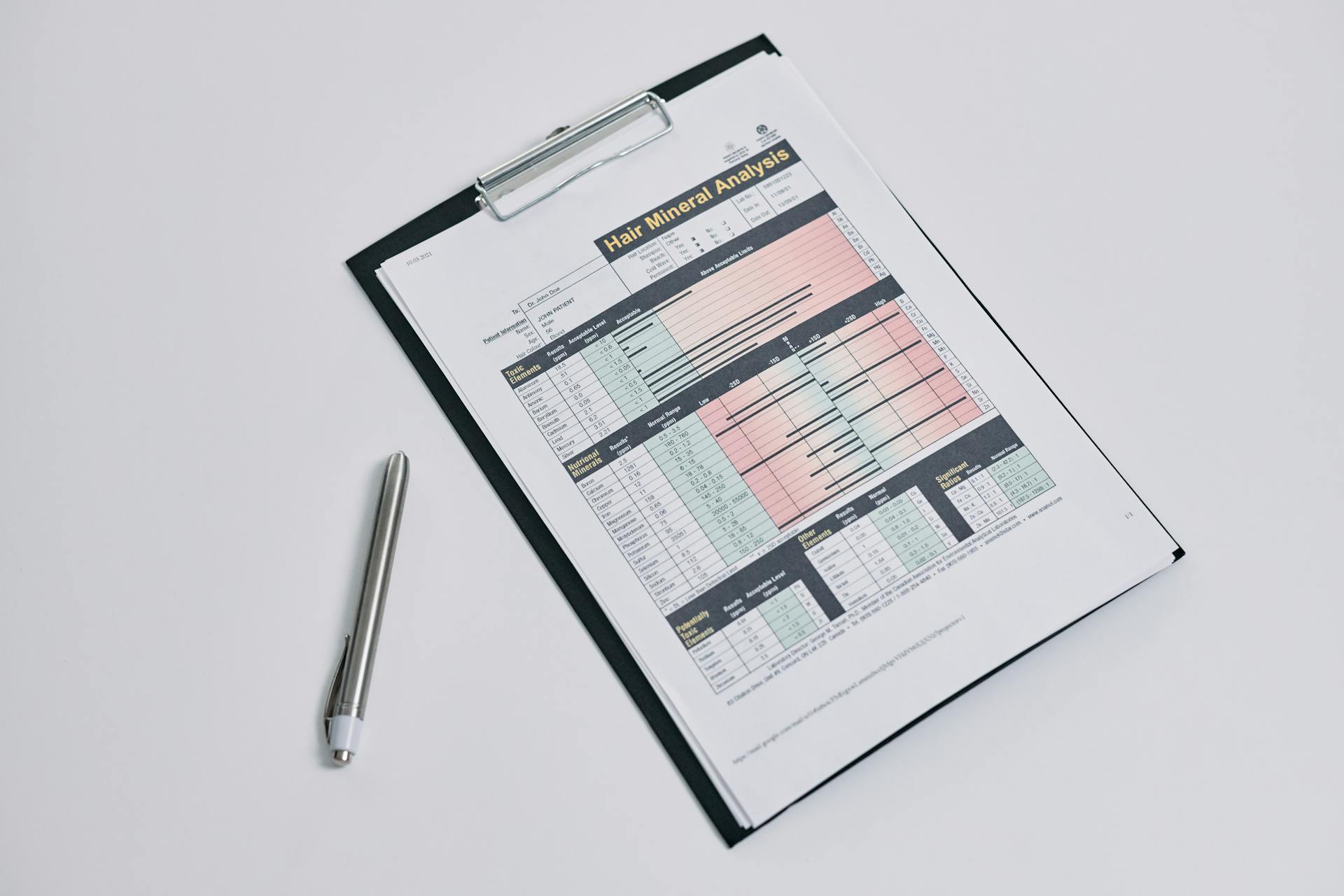
Featured Images: pexels.com


