To get started with Wellpoint prior authorization, you'll need to have your doctor's office contact the insurance company directly. They can reach out to Wellpoint's customer service team at 1-800-899-3084 to initiate the process.
Wellpoint requires prior authorization for certain medications and treatments, which can vary depending on your specific plan and location. You can check your plan documents or contact Wellpoint directly to confirm what's required for your coverage.
Having your doctor's office contact Wellpoint directly can help streamline the process and ensure that everything is handled correctly. This can also help prevent delays in getting the treatment or medication you need.
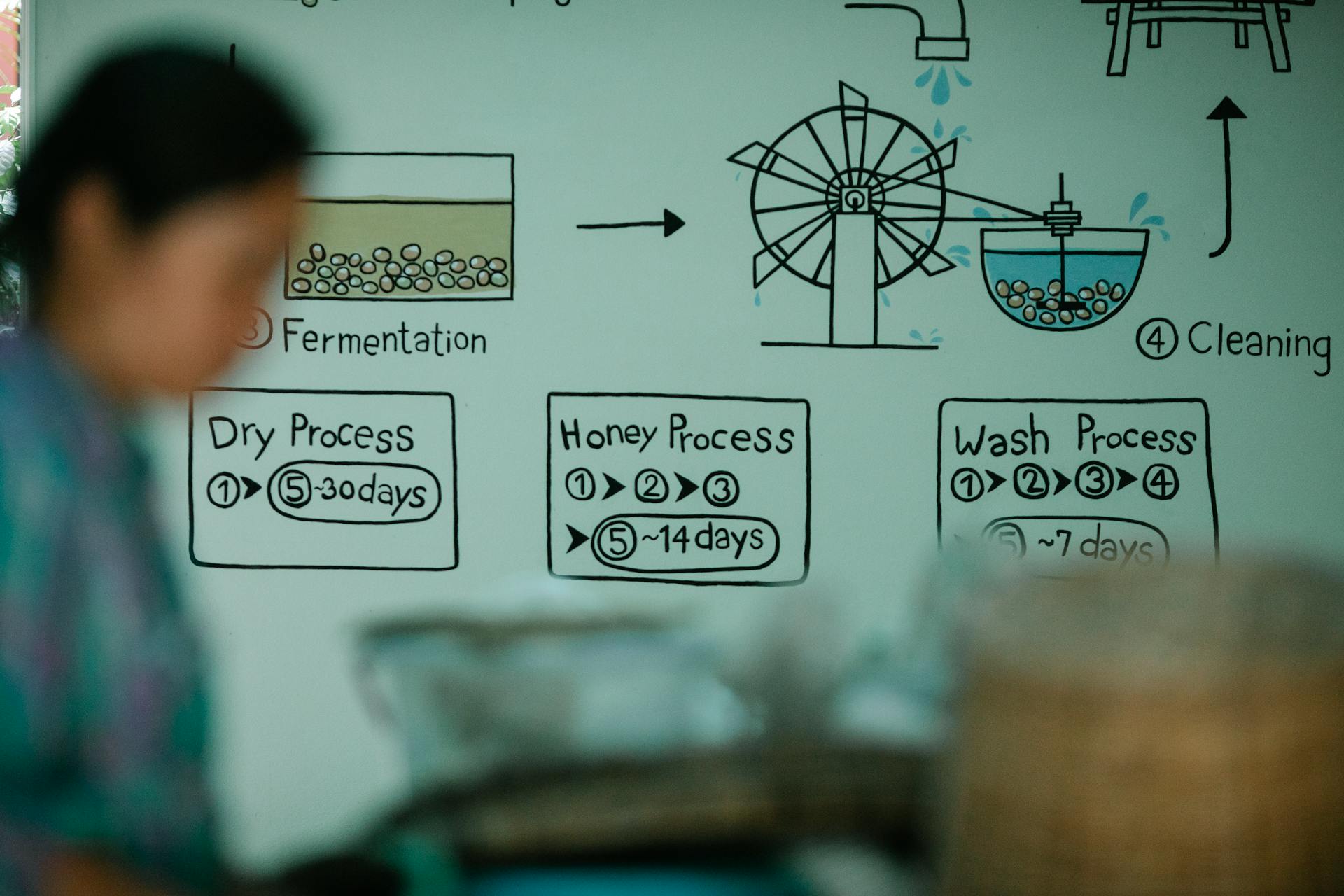
Take a look at this: Prior Authorization Process Flow Chart
Prior Authorization
To initiate a prior authorization request, you can use CoverMyMeds, a free service that streamlines the process. Creating an account is quick and easy.
For medical injectable drugs, you'll need to use the Medical Injectables Prior Authorization Form and include the HCPCS billing code for the injectable drug request.
You can also submit a new PA request by fax or phone. The phone number to call is 1-833-731-2274.
To help you get started, here are the forms you'll need: Pharmacy Retail Prior Authorization FormMedical Injectables Prior Authorization Form
If this caught your attention, see: Gds Claims - Public Adjuster
Prior Authorization Requirements
Prior authorization requirements can be a bit of a hassle, but understanding them can help you navigate the process more smoothly.
Some drugs, drug combinations, and drug doses require prior authorization, which means you need to get approval from the insurance company before they'll cover the cost.
To initiate a new prior authorization request, you can use CoverMyMeds to submit electronic prior authorization requests. Creating an account is free, and it can help streamline the process.
You can also initiate a new PA request by fax or phone, but be aware that some drugs, like medical injectables, require a specific form.
For medical injectable drugs, you'll need to use the Medical Injectables Prior Authorization Form and include the HCPCS billing code for the injectable drug request.
If you need to fax or phone in a request, you can reach out to 1-833-731-2274.
Here are some forms you may need to use for prior authorization:
- Pharmacy Retail Prior Authorization Form
- Medical Injectables Prior Authorization Form
Prior Authorization Status
Prior authorization status can be a major headache, especially if you're not familiar with the process.
The status of your prior authorization request can be checked online or by contacting your health plan directly.
You can usually check the status of your request on your health plan's website or mobile app.
Most health plans update the status of prior authorization requests within 2-5 business days.
It's a good idea to follow up with your health plan if you don't see an update on the status of your request after 5 business days.
Some health plans may require additional documentation or information to process your prior authorization request.
A unique perspective: Health Plans Inc Prior Authorization Form
Sources
- https://www.provider.wellpoint.com/washington-provider/resources/prior-authorization
- https://www.provider.wellpoint.com/iowa-provider/resources/prior-authorization-requirements
- https://www.wellpoint.com/md/provider/state-federal/eligibility-pharmacy/pharmacy
- https://www.provider.wellpoint.com/washington-provider/member-eligibility-and-pharmacy/pharmacy-information
- https://www.wellpoint.com/mass/providers/forms
Featured Images: pexels.com


