Ensuring patient data security and privacy is a top priority for healthcare providers. The Health Insurance Portability and Accountability Act (HIPAA) sets the standard for protecting sensitive patient information.
HIPAA compliance requires covered entities to implement administrative, technical, and physical safeguards to prevent unauthorized access to protected health information (PHI). This includes conducting regular risk assessments to identify vulnerabilities in their systems and processes.
Covered entities must also establish policies and procedures for handling PHI, including procedures for accessing, disclosing, and storing sensitive information.
What Is HIPAA Compliance?
HIPAA compliance is a set of rules and regulations that protect the confidentiality, integrity, and availability of sensitive patient health information. HIPAA stands for the Health Insurance Portability and Accountability Act of 1996, a federal law that was enacted to address concerns about the handling of medical records.
HIPAA compliance applies to healthcare providers, insurance companies, and other organizations that handle protected health information. This includes hospitals, clinics, pharmacies, and medical billing companies.
The law requires covered entities to implement administrative, technical, and physical safeguards to protect electronic protected health information (ePHI). This includes implementing access controls, encrypting data, and monitoring network activity.
Compliance Requirements
HIPAA compliance requirements are a must for all covered entities and business associates who handle Protected Health Information (PHI) in the United States.
To achieve HIPAA compliance, organizations must address the following requirements:
- Administrative Safeguards: This involves developing written policies and procedures related to PHI security and privacy, designating a privacy and security officer, and conducting workforce training on HIPAA regulations.
- Physical Safeguards: This includes controlling access to facilities where PHI is stored, using security cameras and other security measures, and maintaining proper disposal procedures for any PHI-containing devices or media.
- Technical Safeguards: This requires ensuring that ePHI is protected through access controls, such as unique user IDs and passwords, encryption of data at rest and in transit, regular security updates and software patching, and monitoring network activity to identify any unauthorized access or data breaches.
- Breach Notification: In a data breach involving PHI, organizations must follow specific procedures to effectively notify affected individuals and the Department of Health and Human Services.
- Business Associate Agreements: Covered entities must establish agreements with their business associates, including provisions requiring them to adhere to HIPAA regulations.
- Privacy Rule: This enforces how covered entities and their business associates use and disclose PHI, and requires organizations to set policies and procedures to comply with these regulations.
- Security Rule: This requires covered entities and business associates to implement administrative, physical, and technical safeguards to protect ePHI from unauthorized access, use, or disclosure.
By adhering to these HIPAA compliance requirements, organizations can effectively protect patient privacy and maintain the trust of their patients and clients.
Develop Policies and Procedures
Developing policies and procedures is a crucial step in achieving HIPAA compliance. To ensure the security of Protected Health Information (PHI), organizations must implement comprehensive policies that cover all aspects of handling PHI.
Regular review and update of these policies are essential to meet regulatory requirements. This includes reviewing and updating policies to ensure they are aligned with changing regulatory requirements.
To maintain compliance, organizations must develop and implement policies and procedures that outline how PHI is handled, accessed, and disclosed. This includes providing guidance on breach notification procedures and patient rights.
Implementing physical and technical safeguards is not enough; organizations must also have well-defined policies in place. These policies should address the Privacy Rule and Security Rule requirements.
Risk analysis is a critical component of HIPAA compliance. Regular and thorough risk analyses should be conducted to identify infrastructure vulnerabilities, including physical locations where PHI is stored and technical safeguards like encryption methods.
Regular training on HIPAA regulations and best practices for maintaining data privacy is essential for all employees handling PHI. This can include online courses, workshops, or seminars tailored to the organization's specific needs.
A clear policy outlining breach notification procedures is necessary to ensure a timely response in case of a data breach involving unsecured PHI. This policy should be regularly reviewed and updated to ensure compliance with regulatory requirements.
Here are the key components of a comprehensive HIPAA compliance program:
- Risk Analysis: Regular and thorough risk analyses to identify infrastructure vulnerabilities.
- Training Programs: Regular training on HIPAA regulations and best practices for maintaining data privacy.
- Breach Notification Policy: A clear policy outlining how breaches will be handled.
Protect Patient Data
Protecting patient data is a top priority in HIPAA compliance. You need to safeguard all types of sensitive health data, including demographic information, healthcare requirements, and payment for healthcare requirements.
The Privacy Rule defines protected health information (PHI) as individually identifiable health information that is transmitted or stored by covered entities or their business associates. This can take any form – verbal, electronic, or paper.
To prevent data breaches, you need adequate internal security measures and training, as well as a robust cybersecurity program. This will help protect against unauthorized access, use, or release of PHI.
Here are some key safeguards under the Security Rule for PHI:
- Implementing access control measures
- Establishing mechanisms to authenticate ePHI
- Using encryption and decryption tools
- Introducing audit controls and activity logs
- Enabling automatic log-off for devices and desktops
These safeguards will help you maintain the privacy and security of patient data, which is essential to uphold HIPAA regulations.
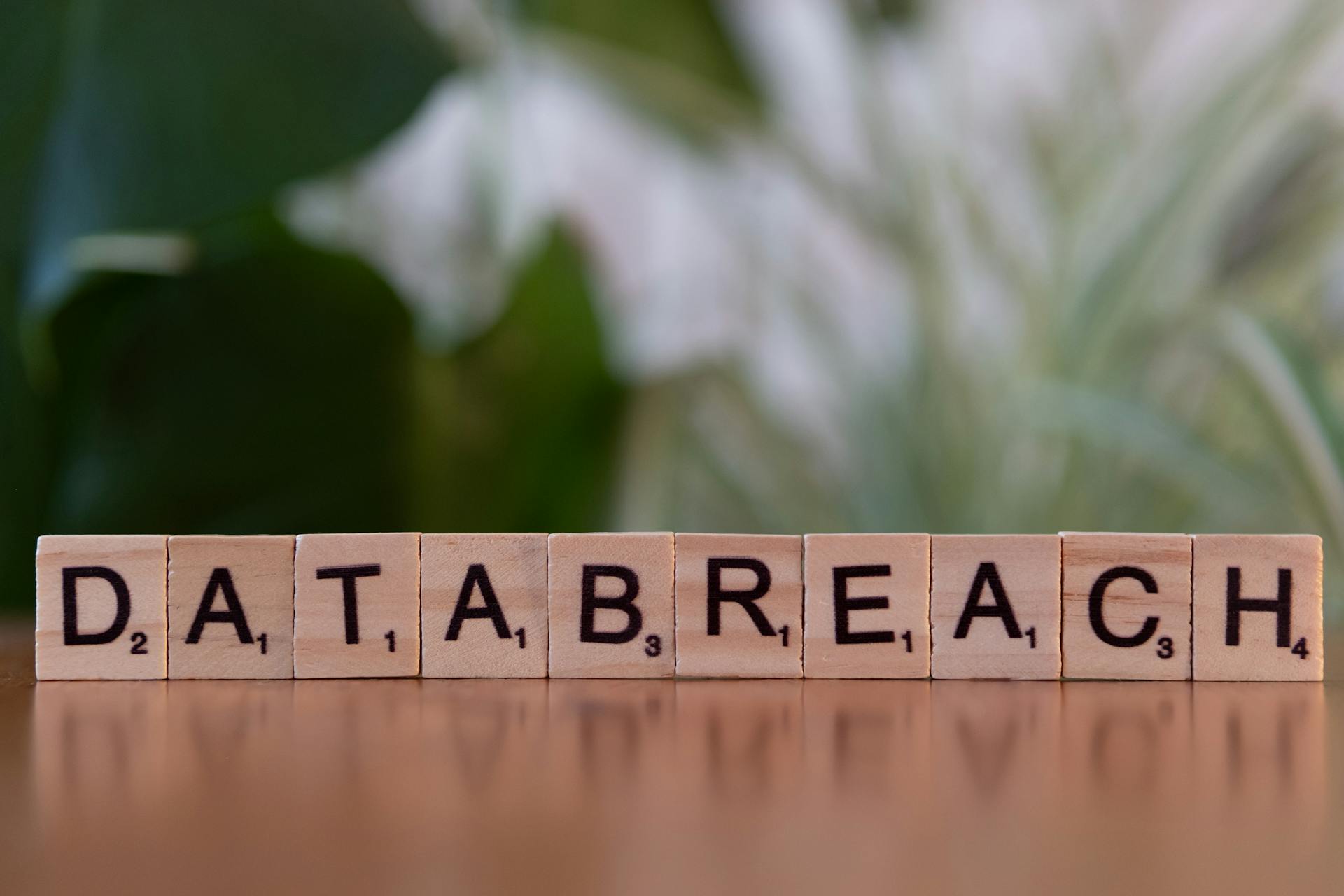
Data Breaches Under
Data breaches under HIPAA can be devastating for individuals and organizations alike. A data breach occurs when protected health information (PHI) is accessed, used, or disclosed without authorization, putting its privacy or security at risk.
According to HIPAA, any unauthorized possession, use, access, or release of PHI is considered a data breach. This can happen through various means, including hacking, phishing, or even internal negligence.
To prevent data breaches, you need to have adequate internal security measures and training, as well as a robust cybersecurity program in place. This includes proper configuration of software like Office 365 for HIPAA compliance.
Data breaches can result in severe consequences, including hefty fines, reputational harm, and legal action. In fact, the largest data breach in history involving PHI was the Anthem, Inc. breach in 2015, which affected nearly 79 million individuals and resulted in a settlement of over $16 million.
Here are some common types of data breaches under HIPAA:
- Unauthorized access or disclosure
- Breach notification failure
- Lack of safeguards
- Poor training
These types of breaches can be prevented by implementing appropriate physical, technical, and administrative safeguards to protect PHI, as well as providing adequate employee training on handling PHI consistent with HIPAA requirements.
Compliance Process
To ensure HIPAA compliance, you need to implement a few key processes. Regular risk assessments and internal audits are essential to evaluate vulnerabilities and threats.
You must perform these audits continuously, not just once, to maintain compliance. This involves monitoring your controls and being prepared for annual audits. Consider a compliance automation solution like Sprinto to make this process easier.
To safeguard Protected Health Information (PHI), you need to implement administrative, physical, and technical measures. This includes access controls, encryption, and backup systems.
Conducting regular audits, reviews, and assessments is crucial to identify vulnerabilities and areas for improvement. This process should include technical risk assessments and reviews of existing contractual agreements regarding HIPAA.
Here are the key steps to ensure HIPAA compliance:
- Implement internal audits and risk assessments.
- Establish a practice of continuous monitoring.
- Deploy security safeguards, such as access controls and encryption.
- Conduct regular audits and reviews to identify vulnerabilities.
By following these steps, you can ensure ongoing adherence to HIPAA regulations and protect patient data.
Training and Education
Training and education are crucial components of HIPAA compliance. You need to train your staff according to HIPAA guidelines to ensure they understand the regulations.
HIPAA compliance relies on employees' understanding and adherence to the regulations, so it's essential to provide comprehensive training on HIPAA laws, updates, and nuances.
Annual training is required for all employees, including trainees, volunteers, employees, or any individual under the direct control of a business associate or covered entity.
Comprehensive training should cover key regulations, updates, and security practices, and should be conducted annually.
Properly educating employees about HIPAA regulations is an essential step for compliance. Organizations should provide training programs to ensure that employees understand their responsibilities, know how to handle PHI securely, and are aware of the potential consequences of non-compliance.
Here are the benefits of HIPAA training:
- Reduces the risk of violations and data breaches due to human error.
- Demonstrates compliance during OCR audits or inquiries.
- Enhances patient trust, supports career advancement, and improves job prospects.
- Minimizes the risk of sanctions, such as written warnings or loss of professional accreditation.
Regulations and Updates
Staying up-to-date with HIPAA regulations is crucial for maintaining compliance.
HIPAA compliance is an ongoing process, so it's essential to stay current with the latest developments.
The recent additions to HIPAA include allowing patients to examine their PHI in person and take notes or photographs, decreasing the maximum time for providing access to PHI from 30 days to 15 days, and requiring entities to publish their fee schedule for PHI access and disclosure on their websites.
You can also find the most recent updates to HIPAA compliance by subscribing to reputable sources such as HIPAA Journal.
The FTC has also updated the Health Breach Notification Rule, which now includes new and revised definitions to expand coverage to health apps and other technologies not covered by HIPAA.
To stay compliant, it's essential to regularly review and update your security policies and procedures to meet the regulatory requirements.
Here are some key updates to be aware of:
- Allowing patients to examine their PHI in person and take notes or photographs
- Decreasing the maximum time for providing access to PHI from 30 days to 15 days
- Requiring entities to publish their fee schedule for PHI access and disclosure on their websites
- Enlarging the definition of healthcare operations to encompass care coordination and case management
Policies and Procedures
Developing effective policies and procedures is a crucial step in achieving and maintaining HIPAA compliance. To ensure the security of Protected Health Information (PHI), organizations must establish comprehensive policies that outline how PHI is handled, accessed, and disclosed.
Regular risk analyses should be conducted to identify infrastructure vulnerabilities, including assessing physical locations where PHI is stored and reviewing technical safeguards like encryption methods.
Clear policies are essential to guide employees on HIPAA regulations and best practices for maintaining data privacy. All employees handling PHI must undergo regular training on HIPAA regulations and best practices.
Organizations must have a breach notification policy in place to ensure timely response and mitigate damage caused by unauthorized disclosure of sensitive information. In case of a data breach involving unsecured PHI, organizations are required by law to notify affected individuals promptly.
A well-defined policy addressing the Privacy Rule and Security Rule requirements is necessary to ensure HIPAA compliance. These policies should be regularly reviewed and updated to meet regulatory requirements.
Here are the key components of effective policies and procedures:
- Risk Analysis: Regular and thorough risk analyses should be conducted to identify infrastructure vulnerabilities.
- Training Programs: All employees handling PHI must undergo regular training on HIPAA regulations and best practices for maintaining data privacy.
- Breach Notification Policy: In case of a data breach involving unsecured PHI, organizations are required by law to notify affected individuals promptly.
Frequently Asked Questions
What are the three rules of HIPAA?
The three main rules of HIPAA are the Privacy Rule, Security Rule, and Breach Notification Rule, which regulate the handling of sensitive patient information. Understanding these rules is crucial for healthcare providers to maintain confidentiality, protect data, and notify patients in case of a breach.
Sources
- https://www.cdc.gov/phlp/php/resources/health-insurance-portability-and-accountability-act-of-1996-hipaa.html
- https://sprinto.com/blog/hipaa-compliance/
- https://online.law.pitt.edu/blog/understanding-hipaa-compliance
- https://www.proofpoint.com/us/threat-reference/hipaa-compliance
- https://www.nist.gov/programs-projects/security-health-information-technology/hipaa-security-rule
Featured Images: pexels.com