
Medicare does cover compression stockings, but with certain conditions. You'll need to have a doctor's prescription to get them covered.
The compression stockings must be prescribed for a medical condition, such as varicose veins or lymphedema. This is a requirement for Medicare coverage.
Compression stockings are considered a durable medical equipment (DME) by Medicare, which means they're covered as part of your medical care.
Insurance Coverage Scenarios
Insurance coverage for compression stockings is typically limited to specific medical conditions where they are deemed medically necessary.
Chronic Venous Insufficiency (CVI) is one such condition, where Medicare may cover compression stockings if you have been diagnosed with it and they are used to treat severe symptoms, particularly open venous stasis ulcers.
After certain surgeries, especially those involving the veins, your doctor might prescribe compression stockings to aid in healing and prevent complications. Medicare might cover these stockings if they are part of your recovery plan.
Medicare has also expanded its coverage to include compression garments for treating lymphedema, starting in 2024. If your doctor prescribes compression stockings as part of your lymphedema treatment, Medicare may cover them under Part B.
Varicose Veins & Lymphedema

Varicose veins are enlarged, twisted veins that can be painful and unsightly. They result from blood pooling in the veins due to faulty valves.
Compression stockings can be a game-changer for managing varicose veins by reducing swelling and alleviating pain. If you have varicose veins, your doctor might prescribe compression stockings to help manage symptoms.
Lymphedema, on the other hand, is a condition where excess lymph fluid builds up in the body's tissues, causing significant swelling, particularly in the arms or legs. This condition is characterized by swelling due to a compromised lymphatic system.
Medicare has expanded its coverage to include compression garments for treating lymphedema starting in 2024. If your doctor prescribes compression stockings as part of your lymphedema treatment, Medicare may cover them under Part B.
Compression stockings can help manage both varicose veins and lymphedema by reducing swelling and alleviating pain. They can also prevent the worsening of symptoms.
Part B
Medicare Part B covers compression stockings under very specific circumstances, such as when used to treat an open venous stasis ulcer. This is because they are considered durable medical equipment (DME) necessary for wound care.
However, for other conditions like varicose veins or general swelling, Medicare Part B does not cover compression stockings, even if prescribed by a healthcare provider.
You would be responsible for paying the full cost out-of-pocket for compression stockings used for these reasons. This can be a significant expense, especially if you need to purchase them regularly.
Medicare Part B only covers 80% of the Medicare-approved amount for compression stockings after you've met your annual deductible of $240 in 2024.
Coverage Exclusions
If you're considering getting compression stockings, it's essential to understand what's not covered by insurance. Specifically, the NIHB program excludes certain types of stockings from coverage.
Compression stockings for comfort or recreational purposes are not eligible for coverage. This includes stockings with a degree of compression lower than 20 mmHg.

If you're looking for medical-grade compression stockings, be aware that non-medical support hosiery, including sport compression socks, is also excluded.
Certain medical conditions, such as acute and active treatment, including edema reduction, DVT, and cellulitis, are not covered by the NIHB program. This means that if you're currently undergoing treatment for one of these conditions, you won't be eligible for coverage.
Prevention, such as thromboembolism-deterrent stockings, is also not covered. Additionally, compression stockings for short-term management (less than 6 months) are excluded from coverage.
Nighttime use of compression stockings is also not covered by the NIHB program.
Getting Legwear Covered
Medicare does not cover compression stockings or socks unless a doctor prescribes them to treat a medical condition.
To get compression stockings covered by Medicare, they must be used to relieve leg pain, prevent blood clots, and minimize swelling.
If you have a Medicare Advantage plan, it may also provide coverage for compression stockings.
How to Get Legwear Covered

To get legwear covered, you'll need a doctor's prescription. Medicare typically doesn't cover compression stockings or socks unless they're prescribed to treat a medical condition.
If you have a Medicare Advantage plan, it may provide additional coverage for compression stockings. However, you'll still need a doctor's prescription for them to be covered.
Medicare Part B may cover compression stockings if they're prescribed to treat specific conditions like open venous stasis ulcers. But for other conditions, you may need to explore alternative insurance options.
Your Medicare insurance company will check if your compression stockings are covered, but only if a doctor prescribes them to treat a medical condition.
How Often Can I Get New Clothes?
Getting new clothes can be a hassle, especially if you're relying on insurance to cover the cost. Under Medicare, you can get new compression garments every 6 months for daytime use.
This means you can swap out your daytime compression gear every 6 months, which is a relatively short timeframe. You can get new compression garments every 2 years for nighttime use.
If your condition changes, or if your compression garments are lost, stolen, or damaged, Medicare may cover replacements. This is a big relief if you're not able to afford new compression garments on your own.
Frequently Asked Questions
Can a doctor write a prescription for compression socks?
A doctor can provide a prescription for compression socks if you have a medical reason for wearing them, and a medical professional will help with the fitting. A prescription is typically required for custom-fit compression socks.
What diagnosis covers compression stockings?
Lymphedema diagnosis is required for coverage of compression stockings under Part B (Medical Insurance). Your doctor's prescription is also necessary for coverage.
Sources
- https://themedicarefamily.com/blog/does-medicare-cover-compression-stockings/
- https://www.absolutemedical.com/medicare-policy-for-compression-garments/
- https://www.sac-isc.gc.ca/eng/1585322780192/1585322799216
- https://pubmed.ncbi.nlm.nih.gov/12021694/
- https://medicarehope.com/medicare-cover-compression-stockings/
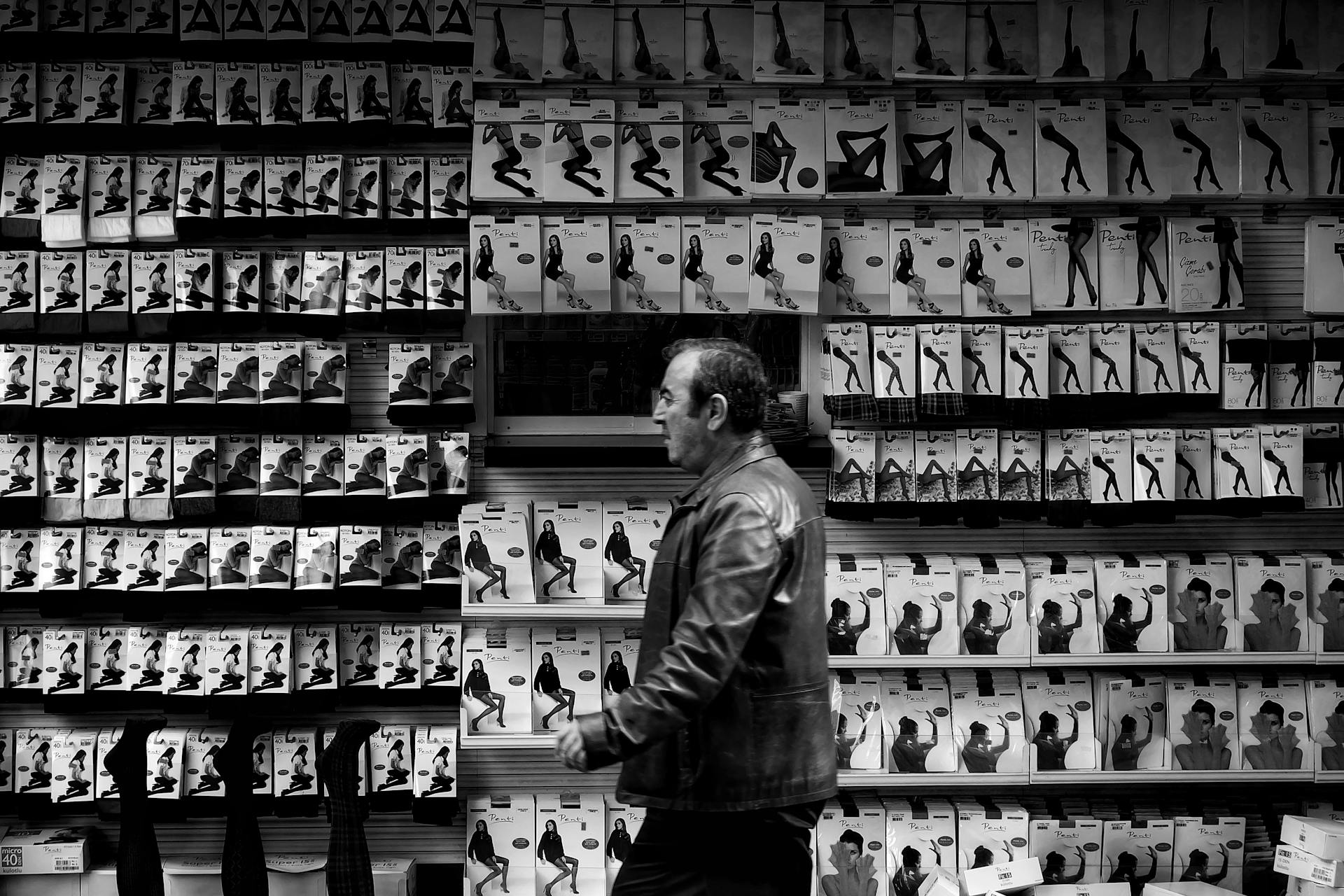
Featured Images: pexels.com

