
Insurance coverage for breast implants can be a complex and confusing topic for trans women.
In the United States, the Affordable Care Act (ACA) requires health insurance plans to cover mastectomy, which includes the removal of breast tissue, but not breast reconstruction.
Some health insurance plans may cover breast reconstruction, including breast implants, as an additional procedure.
Most insurance plans will require a letter from a healthcare provider stating that breast implants are medically necessary for the individual's transition.
You might enjoy: Does Insurance Cover Fat Grafting for Breast Reconstruction
Insurance Coverage
Insurance companies can't deny coverage by deeming gender-affirming surgeries cosmetic, as major medical groups acknowledge their medical necessity.
Transgender patients have more legal rights and protections today than in the past, making it harder for insurance companies to deny coverage.
Medicare and Medicaid started providing some coverage for transgender healthcare in 2014, although decisions are still made on a case-by-case basis.
You should refer to your health plan's handbook and medical policy listing to review their coverage for transgender-specific care, as this will give you a rough idea of how much of the cost your insurance will cover.
Insurance providers can find ways to bypass legal regulations, so it's essential to know your legal rights if your claim is denied.
Recommended read: Bcbs Illinois Transgender
Cost of Surgery
Applying for preauthorization can help secure coverage for your breast implant surgery, but not every plan allows or requires this. This formal process can give you and your medical team a clearer picture of whether insurance will cover your treatment plan.
Most plans will require you to write a letter for preauthorization that explains your treatment plan and why it's medically necessary. Your medical team can help you with this step.
You may need to make a case for your treatment being medically necessary, and different insurance plans will require different information to be included. There are online resources available, such as templates from Transequality.org, that can help guide you through this process.
In some cases, you'll be told that preauthorization isn't necessary because the procedure is covered under your plan. However, it's still a good idea to go through the process to ensure you understand your financial responsibility.
It's worth noting that insurance companies can't deny coverage by deeming gender-affirming surgeries cosmetic, thanks to stronger legal protections for transgender patients.
Procedure and Planning

The procedure for top surgery, also known as breast augmentation or reduction, can be complex due to anatomical differences between male and female chests.
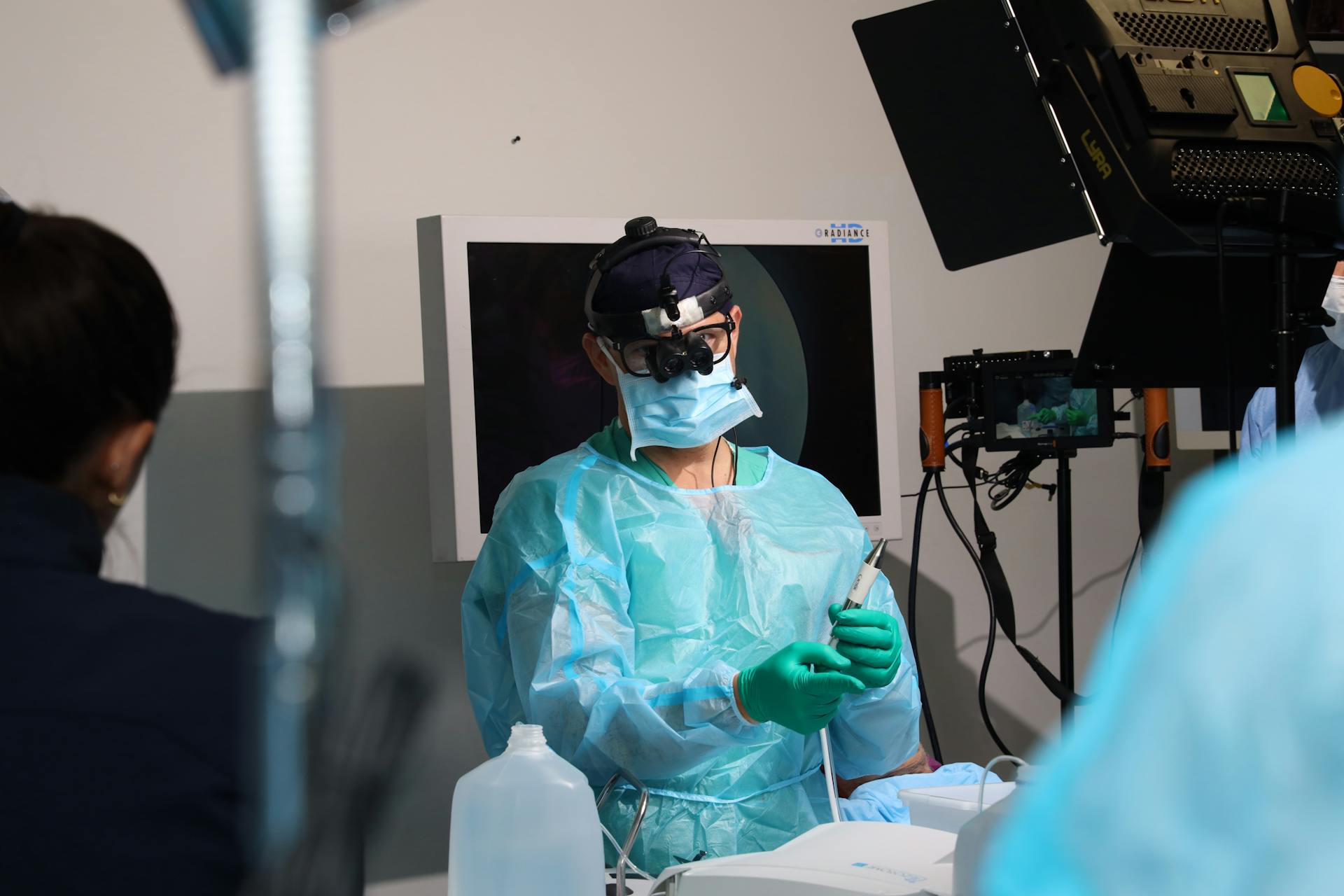
Board-certified plastic surgeons like Dr. Elliot Hirsch specialize in both cosmetic and reconstructive breast surgery, and will work with patients to achieve their best possible result.
The type of procedure and number of stages will depend on the patient's individual needs, such as skin elasticity and desired implant size.
Male to female (MTF) transgender patients may undergo one or two-stage procedures, with one stage involving the insertion of a tissue expander that is inflated over time to stretch the skin.
Fat grafting can be performed during either one or two-stage procedures.
Female to male (FTM) transgender patients typically undergo a combination of skin removal and breast tissue removal, often using breast reduction techniques to flatten the breast and reposition the nipple.
Both male to female breast augmentation and female to male breast reduction can be performed as outpatient procedures, allowing patients to go home the same day.
Most patients experience minimal discomfort and soreness, and are able to resume their regular activities within 2-4 weeks.
Explore further: Does Insurance Cover Ear Cleaning
Frequently Asked Questions
How to get breast implants covered by insurance?
Breast implants are typically covered by insurance when used for reconstructive surgery after a mastectomy, as part of breast cancer treatment. Check with your insurance provider to see if they cover mastectomy and breast cancer treatment, which may qualify you for coverage.
Can a boob job be medically necessary?
Breast implants for cosmetic purposes are not considered medically necessary, but complications from these procedures may be covered under California law.
Sources
- https://transhealthproject.org/resources/health-insurance-medical-policies/views/breast-reconstruction/
- https://www.denverhealth.org/services/lgbtq-services/gender-affirming-surgery/breast-construction-surgery
- https://www.leifrogersmd.com/blog/transgender-surgery-cost-how-to-get-insurance-coverage/
- https://www.hirschplasticsurgery.com/treatments/breast/transgender-breast-surgery/
- https://www.healthpartners.com/blog/gender-affirming-care-covered-by-insurance/
Featured Images: pexels.com


