
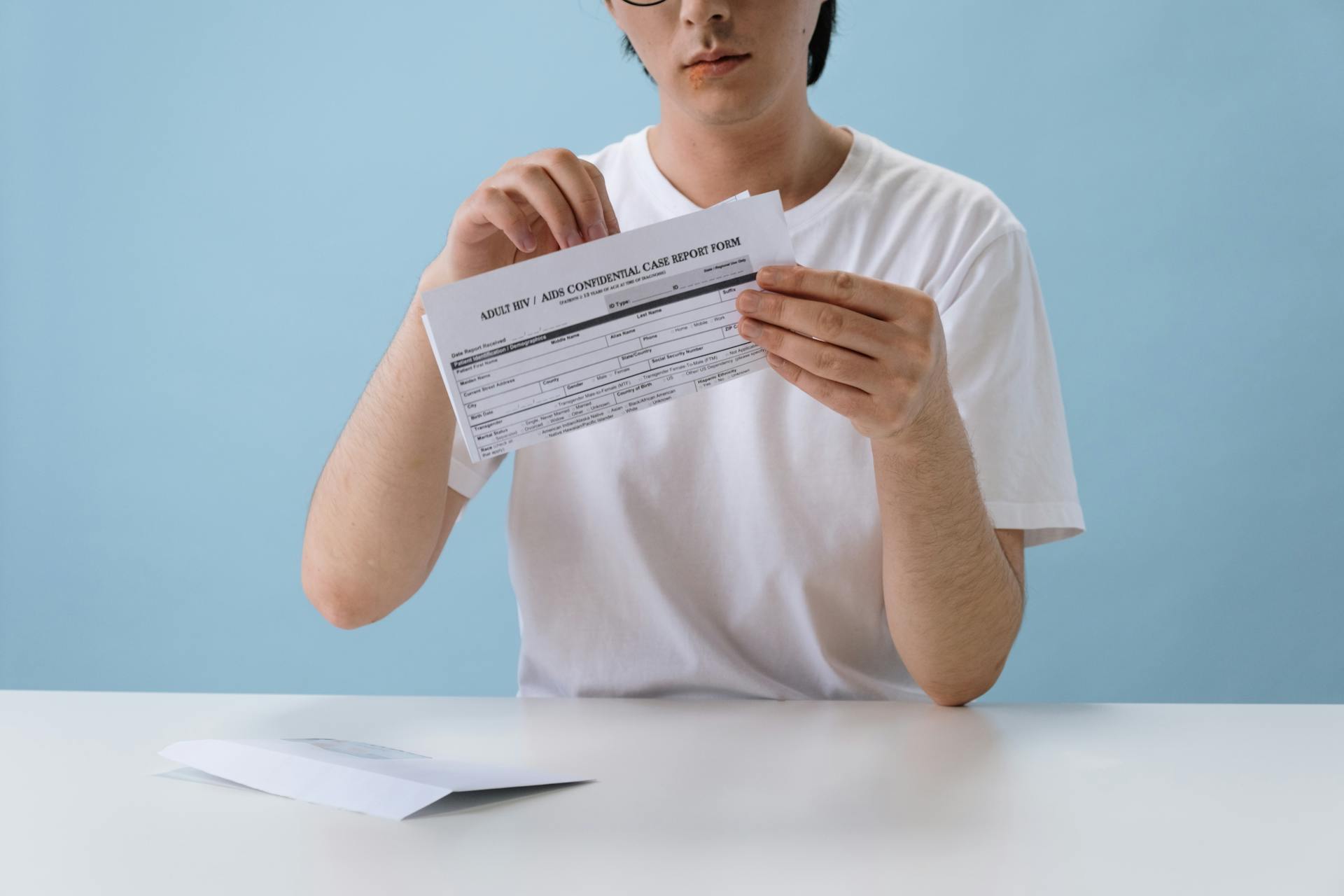
Navigating the BCBS Medicare prior authorization form can be a daunting task, but with the right guidance, you can achieve success.
The form is usually 2-4 pages long and requires detailed information about the patient's condition, treatment plan, and medical history.
To start, gather all necessary documents, including the patient's ID, medical records, and treatment plans.
A typical form will ask for the patient's name, date of birth, and Medicare ID number.
Curious to learn more? Check out: Does Insurance Cover Ed Treatment
Prior Authorization Process
The prior authorization process for BCBS Medicare can be a bit lengthy, but understanding the steps can make it more manageable.
To start, BCBS Medicare requires prior authorization for certain medications and services, including those that are considered high-cost or high-risk.
You can submit a prior authorization request through the BCBS Medicare website, by phone, or through a healthcare provider.
The request must include the patient's information, the medication or service being requested, and the healthcare provider's information.
BCBS Medicare typically reviews prior authorization requests within 24 to 48 hours, but this timeframe may vary depending on the complexity of the request.
If the request is approved, the patient will receive a notification and can proceed with treatment.
Related reading: Bcbs Provider Dispute Form
Understanding BCBS Medicare Plans
BCBS Medicare Plans are offered by Blue Cross and Blue Shield Association, a national organization of independent health insurance companies.
There are several types of BCBS Medicare Plans, including Medicare Supplement Insurance (Medigap) and Medicare Advantage plans.
Medigap plans are designed to fill gaps in Original Medicare coverage, and BCBS offers Plan A, Plan C, and Plan F, among others.
Medicare Advantage plans, on the other hand, are offered by private insurance companies like BCBS and provide an alternative to Original Medicare.
BCBS Medicare Advantage plans often include additional benefits, such as dental, vision, and hearing coverage, as well as fitness programs.
These plans can also offer lower out-of-pocket costs and a network of healthcare providers.
Recommended read: Medigap Meaning
Navigating BCBS Systems
If you're a healthcare provider working with BCBS, navigating their systems can be overwhelming. You'll need to use NaviNet to enter prior authorization requests, access member eligibility and status, and view claims.
To get started, log on to the BCBS payer-provider portal NaviNet. From there, you can receive news alerts in real-time, view member information, submit authorization requests, and check the status of claims.
A unique perspective: Bcbs Medicare Advantage Provider
You can find detailed information on using NaviNet in the NaviNet Medical Authorizations Participant Guide (PDF) and the NaviNet Medical Authorizations Frequently Asked Questions (PDF).
To use NaviNet effectively, you'll want to familiarize yourself with its features. Here are some key things to know:
- You can submit authorization requests electronically through NaviNet.
- You can view gaps in care reports and check the status of claims.
- You can receive auto approvals in some circumstances.
- You can submit amended authorization requests.
- You can attach supplemental documentation.
- You can sign up for in-app status change notifications.
To access the NaviNet Medical Authorizations portal, go to the Workflows menu. From there, you can submit and inquire on existing authorizations, verify if no authorization is required, and more.
Here are some key features of the NaviNet Medical Authorizations portal:
Special Requirements and Exceptions
If you have a life-threatening condition, you'll need to submit a prior authorization request to BCBS Medicare, which typically takes 24 to 48 hours to process.
In some cases, BCBS Medicare may waive the prior authorization requirement for certain services, such as emergency room visits or hospital stays, if they're deemed medically necessary.
Certain medications, like those used to treat cancer or HIV, may not require prior authorization, but this can vary depending on your specific situation.
If you're receiving care from a specialist, you may need to provide additional information to support your prior authorization request, such as test results or medical records.
BCBS Medicare may also require prior authorization for certain durable medical equipment, like wheelchairs or oxygen tanks, if they're not considered medically necessary.
Frequently Asked Questions
Is prior authorization required for Medicare?
Prior authorization is rarely needed for Medicare services, but exceptions may apply for certain items like prosthetics and durable equipment. Check your coverage for specific details on what's pre-approved and what requires prior authorization.
Does Bluecross Blueshield of Tennessee require prior authorization?
Yes, BlueCross BlueShield of Tennessee requires prior authorization for certain procedures, services, and medications, as well as all inpatient admissions. Check our website for a list of specific requirements and the prior authorization process.
Sources
- https://www.bcbsri.com/providers/preauthorization
- https://www.floridablue.com/members/tools-resources/prior-authorization-medical-services
- https://www.blueshieldca.com/en/provider/authorizations/authorization-forms
- https://www.mibluecrosscomplete.com/providers/prior-authorization-resources/
- https://www.bcbsil.com/provider/claims/claims-eligibility/utilization-management/prior-authorization
Featured Images: pexels.com


